Toxicology findings carry immense weight in determining public health decisions, legal outcomes, and individual futures. Ethical handling of sensitive data demands rigorous protocols, transparency, and unwavering commitment to scientific integrity.
🔬 Understanding the Stakes: Why Toxicology Ethics Matter
Toxicology laboratories operate at the intersection of science, law, and human welfare. When a toxicologist discovers unexpected substances in blood samples, detects lethal concentrations of compounds, or identifies patterns suggesting intentional poisoning, the implications ripple far beyond the laboratory walls. These findings can determine criminal convictions, workplace terminations, child custody battles, insurance claims, and public health interventions.
The ethical responsibility begins with recognizing that every result represents a human story. Behind each sample lies an individual whose life trajectory may fundamentally shift based on how professionals handle, interpret, and communicate toxicological data. This profound responsibility requires establishing comprehensive ethical protocols that protect both scientific integrity and human dignity.
⚖️ The Foundation: Core Ethical Principles in Toxicology
Ethical toxicology practice rests on several foundational principles that guide decision-making when handling sensitive findings. These principles have evolved through decades of professional experience, legal precedents, and scientific consensus.
Confidentiality as Cornerstone
Patient confidentiality stands as the primary ethical obligation in toxicology. Toxicologists must establish robust data protection systems that prevent unauthorized access to sensitive findings. This extends beyond simple password protection to encompass comprehensive information security frameworks.
Laboratory information management systems should implement role-based access controls, ensuring that only authorized personnel view specific results. Audit trails must track every interaction with sensitive data, creating accountability throughout the testing process. When toxicology findings reveal illegal substance use, undisclosed medications, or other potentially damaging information, the professional must navigate the delicate balance between confidentiality and mandatory reporting requirements.
Accuracy and Quality Assurance
Ethical practice demands uncompromising commitment to analytical accuracy. False positive results can destroy careers, relationships, and reputations. False negatives may allow dangerous exposures to continue unchecked or permit guilty parties to escape accountability.
Gold standard protocols require confirmation testing for all positive screening results. Initial immunoassay screens, while efficient for high-volume testing, are susceptible to cross-reactivity and interference. Confirmatory testing using gas chromatography-mass spectrometry or liquid chromatography-tandem mass spectrometry provides definitive identification and quantification.
🎯 Critical Decision Points: When Findings Challenge Ethics
Toxicologists regularly encounter scenarios where ethical pathways are not immediately clear. These decision points require careful consideration of competing obligations and potential consequences.
Unexpected Findings in Clinical Settings
Consider a scenario where routine preoperative testing reveals cocaine metabolites in a patient scheduled for urgent cardiac surgery. The surgeon needs to know about substances that could interact with anesthesia, yet disclosure might stigmatize the patient or lead to altered care based on substance use rather than medical need.
Ethical protocols dictate that clinically relevant findings must be communicated to the treating physician promptly. However, the toxicologist should provide context, including the timeframe of use, approximate concentrations, and clinical significance. This approach respects patient autonomy while ensuring medical safety.
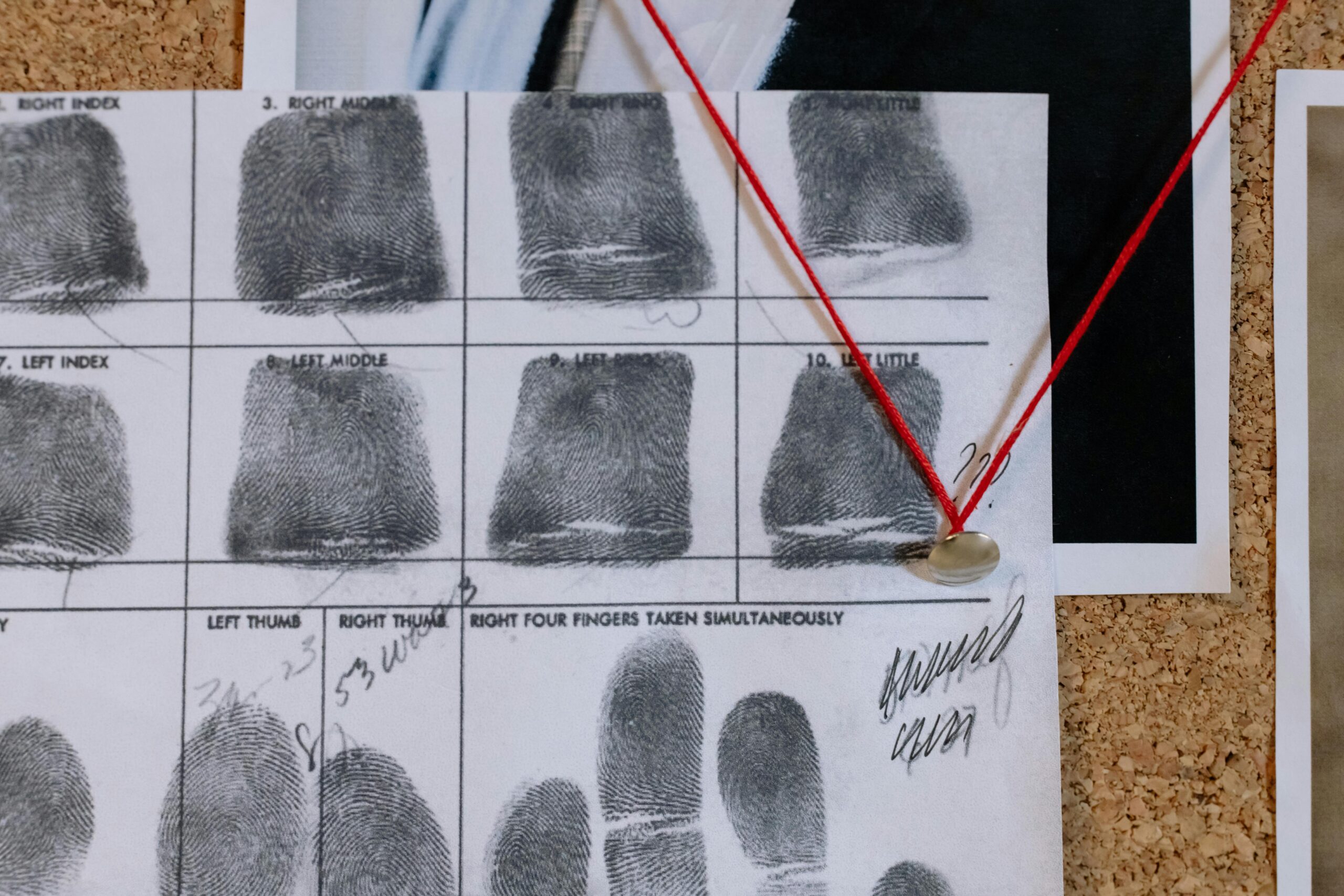
Forensic Toxicology and Legal Implications
Forensic toxicologists face unique ethical challenges when findings could determine criminal prosecution or exoneration. The professional must resist external pressure from law enforcement, attorneys, or other stakeholders seeking specific outcomes.
Chain of custody documentation must be meticulous and unbroken. Any deviation, contamination risk, or procedural irregularity requires transparent disclosure, even when such honesty might weaken a prosecution case or complicate an investigation. The toxicologist’s allegiance is to scientific truth, not to any party’s desired outcome.
📋 Implementing Gold Standard Protocols
Establishing ethical frameworks requires translating principles into concrete operational procedures. Leading toxicology laboratories implement structured protocols that guide staff through complex ethical situations.
Standard Operating Procedures for Sensitive Results
Laboratories should develop detailed SOPs addressing how staff handle high-stakes findings. These procedures should specify:
- Who receives notification of critical results and through what communication channels
- Required documentation for every step of the analytical process
- Procedures for verifying patient identification to prevent misattribution
- Protocols for handling results that may trigger mandatory reporting obligations
- Guidelines for maintaining professional boundaries when findings affect known individuals
- Procedures for addressing potential conflicts of interest
The Verification Imperative
Before releasing sensitive findings, gold standard practice requires multiple verification checkpoints. A second analyst should independently review chromatograms and calculations. Supervisory review adds another quality layer, particularly for results with significant consequences.
This multi-level verification system catches human errors, instrument malfunctions, and interpretation mistakes before results reach stakeholders. While this process requires additional time and resources, the ethical obligation to accuracy justifies this investment.
🤝 Communicating Findings: The Art of Ethical Disclosure
How toxicologists communicate sensitive findings matters as much as analytical accuracy. The ethical professional recognizes that raw data requires context, interpretation, and appropriate framing to be meaningful and fair.
Contextualizing Results
A positive result for a medication may indicate therapeutic use, abuse, or incidental exposure. Reporting simply “positive” without interpretive context can be misleading. Ethical reporting includes:
- Quantitative concentrations rather than just qualitative positive/negative results
- Reference ranges indicating therapeutic, toxic, and lethal levels when applicable
- Discussion of possible alternative explanations for findings
- Acknowledgment of test limitations and potential sources of error
- Recommendations for additional testing when initial results are ambiguous
Appropriate Recipients
Ethical protocols strictly define who may receive toxicology results. In workplace drug testing, results should go to the medical review officer, not directly to employers. In clinical settings, results belong to the ordering physician, not to family members or other parties.
When legal subpoenas demand disclosure, toxicologists should verify the subpoena’s validity and consult with legal counsel before releasing information. Patient authorization should be confirmed whenever possible, respecting autonomy even within legal constraints.
🛡️ Protecting Against Bias and Discrimination
Toxicology findings can reinforce societal biases and discrimination if not handled with awareness and care. Ethical professionals actively work to prevent their findings from being misused to stigmatize vulnerable populations.
Recognizing Systemic Inequities
Drug testing disproportionately affects lower-income workers, minorities, and individuals in certain professions. A positive marijuana test may cost a warehouse worker their job while a corporate executive faces no workplace testing. Toxicologists cannot solve these systemic inequities, but they can ensure their practices do not exacerbate them.
This means applying identical analytical standards regardless of the sample source, providing equally thorough interpretive comments for all results, and advocating for fair policies within one’s sphere of influence.
Challenging Inappropriate Requests
Ethical toxicologists must be prepared to decline requests that violate professional standards. This includes refusing to alter results to match desired outcomes, declining to perform testing without proper authorization, and pushing back against rushed timelines that compromise quality.
These conversations can be difficult, particularly when stakeholders hold power over contracts or institutional relationships. Professional societies and regulatory bodies provide support for toxicologists facing pressure to compromise ethics.
🔄 Continuous Improvement: Learning from Ethical Challenges
Ethical practice evolves through reflection, discussion, and systematic review of challenging cases. Leading laboratories establish ethics committees or regular case conferences where staff can discuss difficult situations in a confidential setting.
Case Review Sessions
Regular meetings to review ethically complex cases help staff develop judgment and ensure consistent approaches. These sessions might examine situations like:
- How to handle discrepancies between patient-reported medication lists and analytical findings
- Balancing confidentiality when findings suggest risk to third parties
- Responding to external pressure to expedite or alter results
- Addressing situations where financial considerations conflict with ethical obligations
Professional Development
Ongoing ethics training should be mandatory for all laboratory personnel handling toxicology samples. This training extends beyond initial orientation to include regular updates on emerging ethical challenges, legal developments, and best practices.
Professional certifications in toxicology increasingly incorporate ethics components, recognizing that technical competence alone is insufficient for responsible practice. Toxicologists should pursue continuing education in bioethics, research ethics, and professional responsibility.
📱 Technology’s Role in Ethical Practice
Modern laboratory information systems can reinforce ethical protocols through technological safeguards. Properly designed systems prevent results from being altered after initial entry, maintain comprehensive audit trails, and flag unusual patterns requiring supervisory review.
Automated decision support can help identify results requiring confirmation testing, flag clinically critical values for immediate communication, and ensure mandatory reporting obligations are met. However, technology cannot replace professional judgment in navigating complex ethical situations.
🌐 Global Perspectives: Cultural Considerations in Toxicology Ethics
Ethical frameworks must adapt to diverse cultural contexts while maintaining core principles. Attitudes toward substance use, privacy expectations, and authority relationships vary significantly across cultures.
Toxicologists working in international contexts or with diverse populations should seek cultural competence training. This includes understanding how different communities view medical testing, confidentiality, and information sharing. Ethical practice requires respecting these differences while upholding fundamental scientific and ethical standards.
💡 Building an Ethical Culture: Institutional Responsibility
Individual ethical behavior flourishes within supportive institutional environments. Laboratory directors and healthcare organizations must create cultures where ethical conduct is expected, recognized, and rewarded.
Leadership Commitment
Institutional leaders set the ethical tone through their actions, resource allocation, and response to ethical challenges. Leaders who prioritize accuracy over speed, who support staff refusing to compromise standards, and who invest in quality systems demonstrate commitment to ethical practice.
This commitment must extend to protecting whistleblowers who report ethical violations, even when such reports create institutional discomfort or financial consequences.
Transparency and Accountability
Ethical laboratories maintain transparency about their procedures, limitations, and performance metrics. Proficiency testing results, accreditation status, and quality indicators should be readily available to stakeholders.
When errors occur, ethical institutions acknowledge them promptly, investigate thoroughly, and implement corrective actions. This transparency builds trust and demonstrates commitment to continuous improvement.
🎓 The Future of Toxicology Ethics
Emerging technologies and evolving social attitudes create new ethical challenges for toxicology professionals. Oral fluid testing, hair analysis, and point-of-care devices offer new capabilities but also raise questions about consent, accuracy, and appropriate use.
Genetic testing that predicts drug metabolism or addiction susceptibility raises profound questions about privacy, discrimination, and determinism. As these technologies become available, the toxicology community must proactively develop ethical frameworks to guide their implementation.
Cannabis legalization creates complex situations where substances are legal for recreational use but prohibited in workplace settings or affect legal proceedings. Toxicologists must navigate these ambiguities with nuance, recognizing that detection of cannabis metabolites provides limited information about impairment or timing of use.

🏆 Excellence Through Ethics: The Professional Imperative
The gold standard for handling sensitive toxicology findings ultimately rests on professional character and institutional culture. Technical protocols, sophisticated instruments, and regulatory compliance provide necessary structure, but ethical practice fundamentally depends on professionals committed to doing what is right even when it is difficult.
This means choosing accuracy over expediency, transparency over convenience, and patient welfare over external pressure. It requires courage to challenge inappropriate requests, wisdom to navigate ambiguous situations, and humility to acknowledge limitations and uncertainties.
The toxicology community honors this commitment through professional codes of ethics, peer accountability, and recognition that our work profoundly affects human lives. Every sample analyzed, every result reported, and every interpretive comment provided carries ethical weight.
As science advances and society evolves, the fundamental principles guiding ethical toxicology practice remain constant: unwavering commitment to truth, respect for human dignity, protection of confidentiality, and recognition of the profound responsibility we carry. These principles constitute the true gold standard against which all practices must be measured.
By embedding these ethical commitments into daily operations, continuing education, institutional policies, and professional culture, the toxicology community fulfills its obligation to science, to justice, and to the individuals whose lives depend on our integrity. This is the essence of ethical excellence in toxicology practice.
Toni Santos is a biological systems researcher and forensic science communicator focused on structural analysis, molecular interpretation, and botanical evidence studies. His work investigates how plant materials, cellular formations, genetic variation, and toxin profiles contribute to scientific understanding across ecological and forensic contexts. With a multidisciplinary background in biological pattern recognition and conceptual forensic modeling, Toni translates complex mechanisms into accessible explanations that empower learners, researchers, and curious readers. His interests bridge structural biology, ecological observation, and molecular interpretation. As the creator of zantrixos.com, Toni explores: Botanical Forensic Science — the role of plant materials in scientific interpretation Cellular Structure Matching — the conceptual frameworks behind cellular comparison and classification DNA-Based Identification — an accessible view of molecular markers and structural variation Toxin Profiling Methods — understanding toxin behavior and classification through conceptual models Toni's work highlights the elegance and complexity of biological structures and invites readers to engage with science through curiosity, respect, and analytical thinking. Whether you're a student, researcher, or enthusiast, he encourages you to explore the details that shape biological evidence and inform scientific discovery.