Biomedical image matching has revolutionized healthcare diagnostics, but it raises critical questions about patient privacy and ethical data handling in our increasingly digital world.
🔬 The Evolution of Biomedical Image Matching Technology
Biomedical image matching represents one of the most significant technological advancements in modern healthcare. This sophisticated process involves comparing medical images—such as MRI scans, CT images, X-rays, and pathology slides—across databases to assist in diagnosis, treatment planning, and medical research. The technology leverages artificial intelligence and machine learning algorithms to identify patterns, detect anomalies, and match similar cases with remarkable precision.
Healthcare institutions worldwide now routinely store millions of medical images in digital repositories. These vast databases enable physicians to compare a patient’s scan with thousands of similar cases, improving diagnostic accuracy and treatment outcomes. However, this technological leap forward brings unprecedented challenges regarding patient privacy protection and ethical data management.
The intersection of advanced imaging technology and data analytics has created an ecosystem where medical images can be processed, shared, and analyzed at scales previously unimaginable. While this benefits medical science tremendously, it simultaneously exposes sensitive patient information to potential breaches, unauthorized access, and misuse.
🔐 Understanding the Privacy Risks in Medical Image Databases
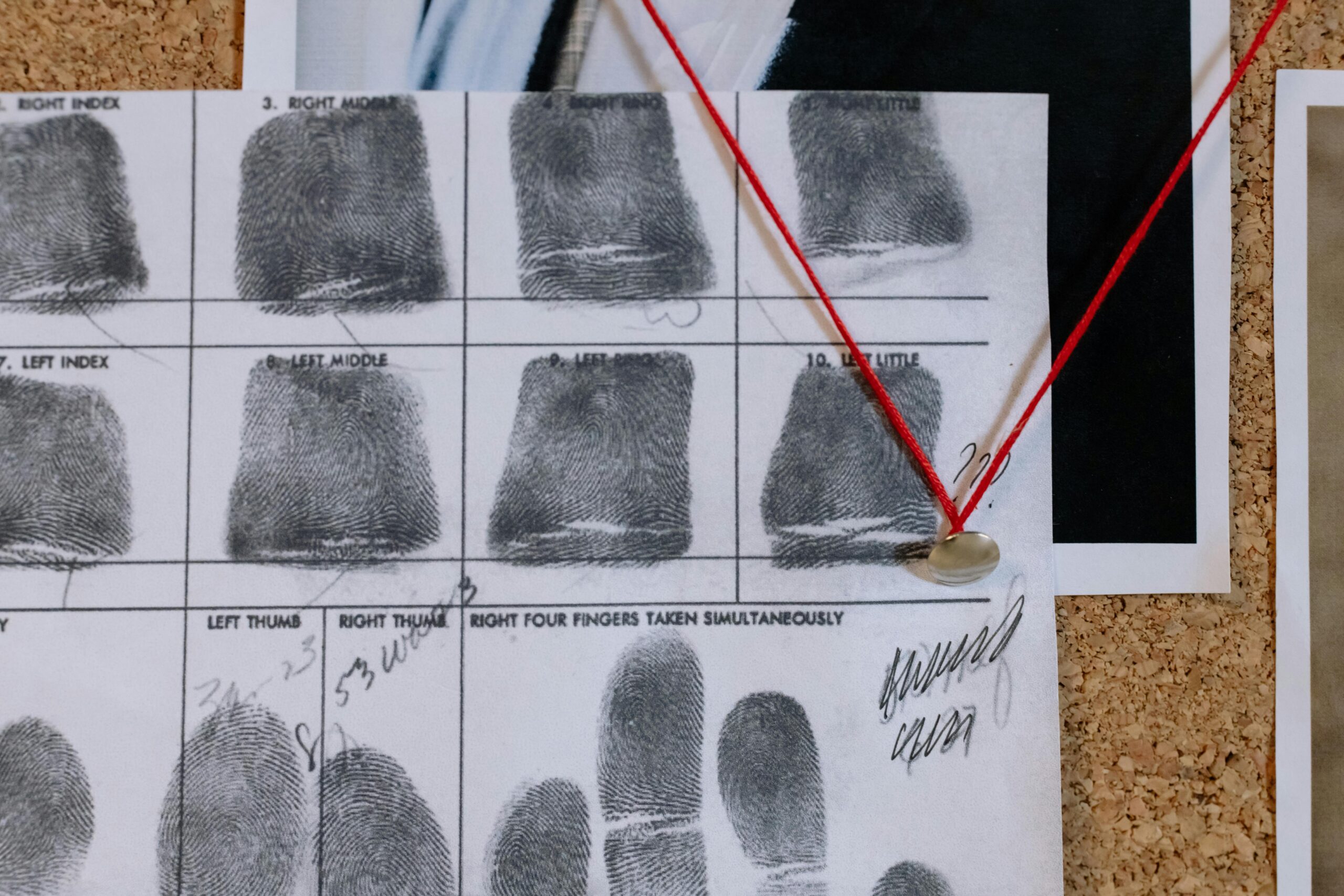
Medical images contain far more identifying information than many people realize. Beyond the obvious patient identifiers like names and dates of birth embedded in DICOM metadata, the images themselves can reveal unique biological characteristics. Facial features in cranial scans, dental patterns, skeletal structures, and even vascular patterns can serve as biometric identifiers capable of re-identifying supposedly anonymized patients.
The privacy risks associated with biomedical image matching extend across multiple dimensions:
- Unauthorized access to sensitive health information revealing diagnoses and conditions
- Re-identification of anonymized patients through advanced imaging analysis techniques
- Data breaches exposing medical records to malicious actors or competitors
- Cross-referencing medical images with public databases for identification purposes
- Commercial exploitation of patient data without proper consent
- Insurance discrimination based on discovered health conditions
These risks become particularly acute when medical images are shared across institutional boundaries, uploaded to cloud-based platforms, or used in collaborative research projects involving multiple stakeholders. Each transfer point represents a potential vulnerability where patient privacy could be compromised.
⚖️ The Ethical Framework for Medical Image Management
Navigating the ethical landscape of biomedical image matching requires balancing several competing interests: advancing medical knowledge, improving patient care, protecting individual privacy, and facilitating legitimate research. This delicate equilibrium rests on fundamental ethical principles that have guided medical practice for centuries, now adapted for the digital age.
The principle of autonomy demands that patients maintain control over their medical information. This means obtaining informed consent before using medical images for purposes beyond direct patient care, ensuring patients understand how their images might be used, stored, and shared. Consent must be specific, informed, and freely given—not buried in lengthy admission paperwork that patients sign without reading.
Beneficence and non-maleficence require healthcare providers to maximize benefits while minimizing harms. In the context of image matching, this translates to implementing robust security measures, using privacy-preserving technologies, and conducting thorough risk assessments before deploying new image matching systems.
Establishing Trust Through Transparency
Trust forms the foundation of the patient-provider relationship, and transparency about data handling practices strengthens this bond. Healthcare institutions must clearly communicate their policies regarding medical image storage, retention periods, access controls, and sharing practices. Patients deserve to know who can view their images, for what purposes, and under what circumstances their data might be shared with third parties.
Transparency also extends to algorithmic decision-making. When AI systems analyze medical images, patients should understand how these algorithms work, what training data was used, and how decisions are made. This transparency enables patients to make informed choices about their care and raises important questions about algorithmic bias and fairness.
🛡️ Technical Safeguards for Privacy Protection
Protecting patient privacy in biomedical image matching requires implementing multiple layers of technical safeguards. These protections must address both external threats from malicious actors and internal risks from unauthorized access by staff members or system vulnerabilities.
Encryption represents the first line of defense. Medical images should be encrypted both in transit and at rest, using industry-standard algorithms that protect data even if storage media is stolen or transmission intercepted. End-to-end encryption ensures that only authorized parties with proper decryption keys can access the actual image content.
De-identification techniques remove direct patient identifiers from medical images and associated metadata. However, simple removal of names and ID numbers proves insufficient given the biometric information inherent in the images themselves. Advanced de-identification employs techniques like:
- Defacing algorithms that obscure facial features in cranial imaging while preserving diagnostic value
- Metadata scrubbing that removes all DICOM tags containing identifying information
- Date shifting that preserves temporal relationships while obscuring actual dates
- Coordinate randomization that prevents spatial re-identification
Emerging Privacy-Preserving Technologies
Cutting-edge privacy technologies offer promising solutions for balancing data utility with privacy protection. Differential privacy adds carefully calibrated noise to datasets, providing mathematical guarantees that individual records cannot be identified while preserving overall statistical patterns. This technique enables researchers to query image databases and extract valuable insights without accessing individual patient images.
Federated learning allows machine learning models to be trained across multiple institutions without centralizing the actual image data. Instead of pooling images in a central repository, the algorithm travels to the data, learns locally, and only shares model updates. This approach dramatically reduces privacy risks while enabling collaborative research on much larger datasets than any single institution possesses.
Homomorphic encryption represents perhaps the most exciting frontier, enabling computations to be performed on encrypted data without decrypting it first. Though computationally intensive, this technology could eventually allow image matching and analysis to occur on fully encrypted datasets, providing ultimate privacy protection.
📋 Regulatory Compliance and Legal Considerations
Healthcare institutions operating biomedical image matching systems must navigate a complex web of privacy regulations that vary by jurisdiction. In the United States, the Health Insurance Portability and Accountability Act (HIPAA) establishes minimum standards for protecting patient health information, including medical images. HIPAA requires covered entities to implement appropriate administrative, physical, and technical safeguards.
The European Union’s General Data Protection Regulation (GDPR) imposes even stricter requirements on organizations handling health data of EU residents. GDPR grants individuals extensive rights over their personal data, including the right to access, correct, delete, and port their information. Medical images constitute particularly sensitive data under GDPR, subject to enhanced protections and requiring explicit consent for processing.
Compliance extends beyond simply meeting minimum legal requirements. Leading healthcare institutions adopt privacy-by-design principles, embedding privacy considerations into every aspect of system architecture from initial conception through deployment and maintenance. This proactive approach proves far more effective than retrofitting privacy protections onto systems designed without adequate consideration for data protection.
🤝 Stakeholder Responsibilities in the Privacy Ecosystem
Protecting patient privacy in biomedical image matching requires coordinated efforts from multiple stakeholders, each bearing distinct responsibilities within the broader privacy ecosystem.
Healthcare Institutions and Providers
Hospitals, clinics, and medical practices bear primary responsibility for implementing robust privacy protections. This includes investing in secure infrastructure, training staff on privacy best practices, conducting regular security audits, and establishing clear policies governing image access and sharing. Providers must also ensure that third-party vendors handling medical images maintain equivalent privacy standards.
Technology Developers and AI Companies
Companies developing image matching algorithms and platforms must build privacy protections into their products from the ground up. This includes implementing strong authentication mechanisms, maintaining detailed audit logs, providing granular access controls, and offering privacy-enhancing features like automatic de-identification. Developers should also conduct thorough testing to identify and mitigate re-identification risks.
Researchers and Academic Institutions
Medical researchers utilizing biomedical image databases must adhere to rigorous ethical standards. Institutional Review Boards should carefully evaluate research protocols involving medical images, ensuring appropriate consent mechanisms, adequate de-identification, and justification for data retention periods. Researchers should also consider using synthetic datasets or privacy-preserving techniques when possible to minimize privacy risks.
Patients and Healthcare Consumers
Patients themselves play a crucial role in protecting their privacy by staying informed about data practices, reading consent forms carefully, asking questions about how their images will be used, and exercising their rights to access and control their medical information. Patient advocacy groups can amplify these concerns and push for stronger privacy protections across the healthcare system.
🌍 Global Perspectives on Medical Data Privacy
Approaches to medical image privacy vary significantly across different cultural and regulatory contexts. Some countries prioritize individual privacy rights above nearly all other considerations, while others emphasize collective benefits and public health interests. Understanding these diverse perspectives enriches the global conversation about ethical data practices.
Scandinavian countries have pioneered comprehensive health registries that link medical data, including images, across entire populations. These systems enable powerful epidemiological research while maintaining strong privacy protections through strict access controls, transparency requirements, and robust oversight mechanisms. The Nordic model demonstrates that population-scale data sharing can coexist with rigorous privacy protection when proper safeguards are implemented.
In contrast, some Asian countries have adopted more flexible approaches that emphasize technological innovation and economic development alongside privacy considerations. China’s rapid advancement in AI-powered medical imaging, for instance, has been enabled partly by access to vast datasets, raising important questions about the appropriate balance between innovation and privacy protection.
🔮 Future Challenges and Emerging Considerations
The landscape of biomedical image matching continues to evolve rapidly, presenting new ethical challenges that require ongoing attention and adaptive solutions. Quantum computing threatens to render current encryption methods obsolete, necessitating development of quantum-resistant cryptographic techniques. As imaging technology advances, producing ever-higher resolution images with more detailed biological information, the risk of re-identification increases correspondingly.
The proliferation of consumer health devices and direct-to-consumer medical imaging services introduces new actors into the privacy ecosystem, often operating under different regulatory frameworks than traditional healthcare providers. These services may offer convenience and lower costs but potentially with reduced privacy protections.
Artificial intelligence systems trained on medical images raise concerns about bias, fairness, and the potential for algorithmic discrimination. If training datasets lack diversity or contain historical biases, AI-powered diagnostic systems may perform poorly for underrepresented populations, creating ethical issues that intersect with privacy concerns.
💡 Best Practices for Ethical Image Matching Implementation
Organizations implementing or upgrading biomedical image matching systems should follow evidence-based best practices that balance innovation with privacy protection:
- Conduct comprehensive privacy impact assessments before deploying new systems
- Implement multi-factor authentication and role-based access controls
- Maintain detailed audit logs of all image access and use
- Establish clear data retention policies with automatic deletion of outdated images
- Provide regular privacy training for all staff with access to medical images
- Engage with patient advisory groups when developing data policies
- Commission independent security audits and penetration testing
- Develop incident response plans for potential data breaches
- Stay current with evolving privacy regulations and technological solutions
These practices should be viewed not as burdensome compliance obligations but as essential components of ethical healthcare delivery and trustworthy institutional stewardship of sensitive patient information.
🎯 Building a Privacy-Conscious Culture in Healthcare
Technical safeguards and regulatory compliance, while necessary, prove insufficient without a broader organizational culture that prioritizes patient privacy. Healthcare institutions must cultivate an environment where every staff member understands their role in protecting patient information and feels empowered to raise concerns about potential privacy violations.
Leadership commitment sets the tone for organizational culture. When executives and senior physicians visibly prioritize privacy, allocate adequate resources for privacy protection, and hold individuals accountable for data breaches, it signals throughout the organization that privacy matters. Conversely, when privacy takes a back seat to efficiency or cost considerations, staff members receive the message that privacy protection is optional rather than essential.
Ongoing education ensures that privacy consciousness remains top-of-mind rather than becoming a checkbox exercise completed during onboarding. Regular training should cover emerging threats, new technologies, updated regulations, and real-world case studies that illustrate the consequences of privacy failures. Interactive training that engages participants proves far more effective than passive consumption of policy documents.

🌟 The Path Forward: Sustainable Privacy Protection
Protecting patient privacy in biomedical image matching represents an ongoing journey rather than a destination. As technology advances and healthcare becomes increasingly data-driven, the ethical landscape will continue to shift, requiring constant vigilance, adaptation, and commitment from all stakeholders.
The healthcare community must resist the false dichotomy between innovation and privacy, recognizing that robust privacy protections ultimately strengthen rather than hinder medical advancement. Patients who trust that their privacy will be respected are more likely to seek care, participate in research, and share information necessary for accurate diagnosis and treatment.
Success requires viewing privacy not as a technical problem to be solved but as a fundamental value to be upheld—an essential component of patient dignity and respect. By embedding privacy considerations into every aspect of biomedical image matching, from system design through clinical implementation and research applications, the healthcare community can harness the transformative potential of this technology while honoring the trust patients place in their care providers.
The challenges are substantial, but so too are the opportunities. With thoughtful attention to ethical principles, investment in privacy-enhancing technologies, robust regulatory frameworks, and genuine commitment to patient welfare, we can navigate the complex ethical landscape of biomedical image matching in ways that advance medicine while preserving the fundamental right to privacy that lies at the heart of humane healthcare.
Toni Santos is a biological systems researcher and forensic science communicator focused on structural analysis, molecular interpretation, and botanical evidence studies. His work investigates how plant materials, cellular formations, genetic variation, and toxin profiles contribute to scientific understanding across ecological and forensic contexts. With a multidisciplinary background in biological pattern recognition and conceptual forensic modeling, Toni translates complex mechanisms into accessible explanations that empower learners, researchers, and curious readers. His interests bridge structural biology, ecological observation, and molecular interpretation. As the creator of zantrixos.com, Toni explores: Botanical Forensic Science — the role of plant materials in scientific interpretation Cellular Structure Matching — the conceptual frameworks behind cellular comparison and classification DNA-Based Identification — an accessible view of molecular markers and structural variation Toxin Profiling Methods — understanding toxin behavior and classification through conceptual models Toni's work highlights the elegance and complexity of biological structures and invites readers to engage with science through curiosity, respect, and analytical thinking. Whether you're a student, researcher, or enthusiast, he encourages you to explore the details that shape biological evidence and inform scientific discovery.